Benign Prostatic Hyperplasia
What is the Prostate?
The prostate is a gland attached to the male genitalia. It is a glandular muscle organ, unique and median, located deeply in the pelvic excavation, under the bladder, above the perineum, ahead of the rectum and behind the pubic symphysis – urogenital junction.
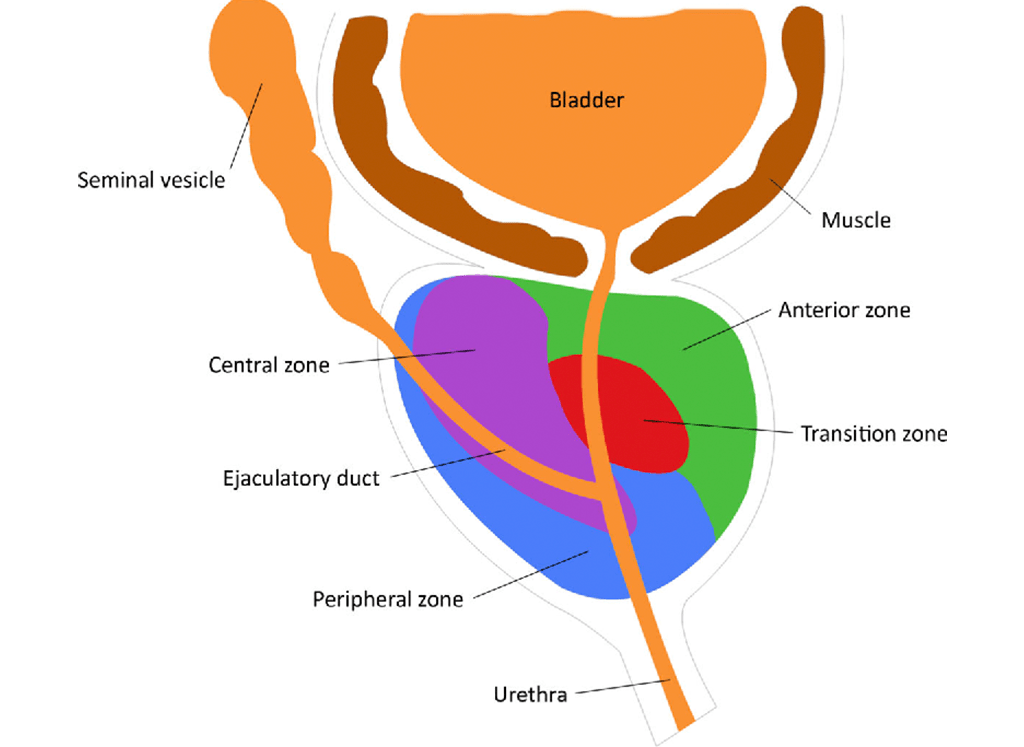
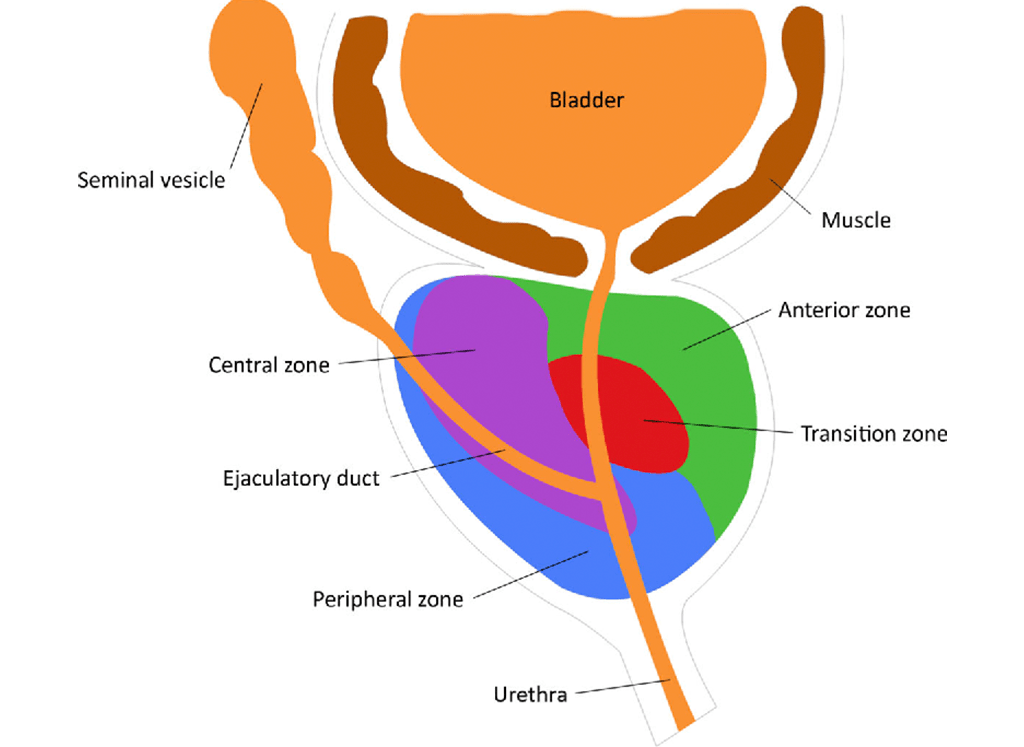
There are 3 main glandular zones in the prostate: central, transitional, and peripheral which are associated with an anterior fibromuscular stroma zone and a periurethral gland zone.
The transitional zone corresponds to 5%-10% of the overall volume and it is adjacent to the proximal urethral sphincter, and it is where most benign prostatic hyperplasia (BPH) develops, as well as 20% of prostate cancer. The peripheral zone is the biggest (70%-80% of glandular tissue) before the increase of the secondary prostatic volume in BPH, and it is the most frequent zone where cancer arises (approximately 70%).
With ultrasound and an MRI, it is possible to observe two distinct prostatic zones. The peripheral zone (corresponds to central and peripheral zones) and central zone (corresponds to transitional zone, periurethral glandular and anterior fibromuscular zone, and internal urethral sphincter), separated by the surgical capsule that becomes more evident when BPH happens with the increase of the transitional zone.
What is Benign Prostatic Hyperplasia (BPH)?
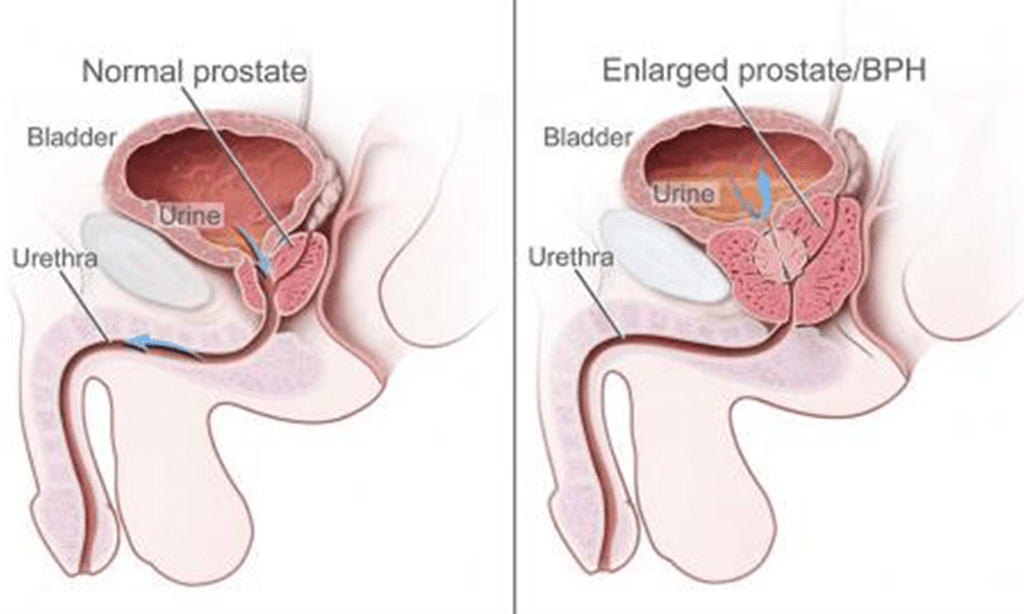
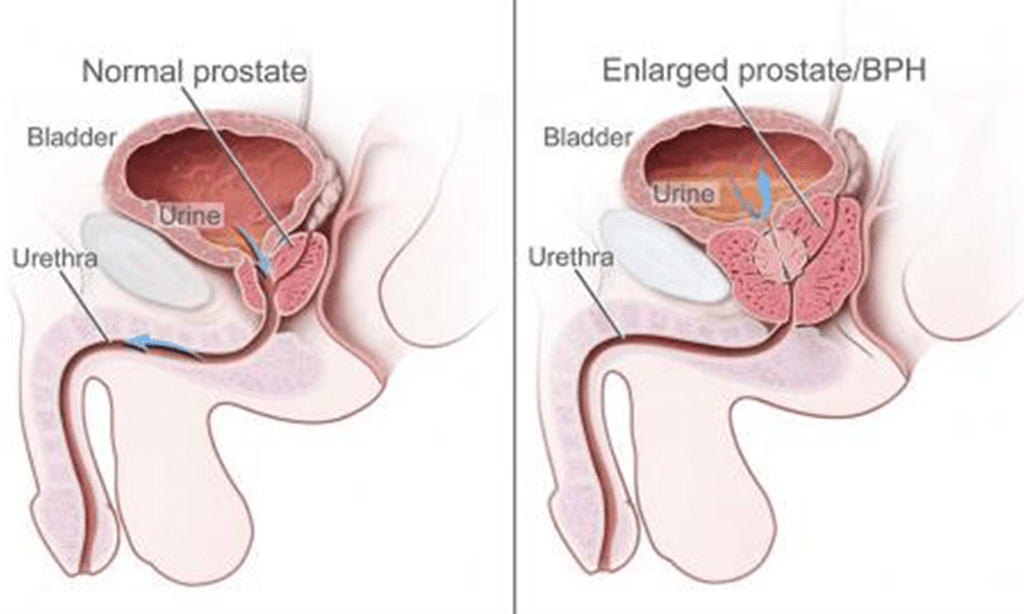
Benign Prostatic Hyperplasia (BPH) is hyperplasia, not hypertrophy, meaning that it is an increase in the number of cells inside the prostate, leading the prostate to increase its size.
Since the prostate is located under the bladder, surrounds the urethra (the tube that empties urine from the bladder), increasing its size can provoke bladder constipation. This way, it usually manifests by difficulties in urinating.
It is a benign disease, not a malignant tumor or cancer. Clinically significant BPH in needing treatment only shows up at 50% of men over 50 years old with increased-dimensions prostates, and it can reach 80% in 80 years old men.
What is Benign Prostatic Hyperplasia (BPH)?
Benign Prostatic Hyperplasia (BPH) is hyperplasia, not hypertrophy, meaning that it is an increase in the number of cells inside the prostate, leading the prostate to increase its size.
Since the prostate is located under the bladder, surrounds the urethra (the tube that empties urine from the bladder), increasing its size can provoke bladder constipation. This way, it usually manifests by difficulties in urinating.
It is a benign disease, not a malignant tumor or cancer. Clinically significant BPH in needing treatment only shows up at 50% of men over 50 years old with increased-dimensions prostates, and it can reach 80% in 80 years old men.
How is Benign Prostatic Hyperplasia (BPH) diagnosed?
The Benign Prostatic Hyperplasia (BPH) diagnosis is usually made based on the prostate-size increase palpation, detected in the clinic or by ultrasound; or for the presence of a set of lower urinary tract symptoms (LUTS), with difficulty in urinating.
Benign prostatic hyperplasia (BPH) is hyperplasia, not hypertrophy. It is known that urinary complaints affect men in a progressive form, especially men over 60 years old whose transitional zone is the most affected.
Although a detailed correlation between urinary complaints, prostate-volume increase, and bladder/urethral constipation is not certain, prostatic embolization in men with benign prostatic hyperplasia (BPH) improves the symptoms, the urodynamic function, and quality of life, reducing the prostate volume.
Benign prostatic hyperplasia (BPH) is a benign disease, not cancer nor a malignant tumor. However, it is an insidious disease that takes many years to develop. It manifests itself through urinary complaints like difficulty to start urinating, urinating several times, waking up in the middle of the night with a compulsion to urinate, urinary burning, failure to empty the bladder, and several others.
These complaints are progressive and keep getting worst with age, but they frequently lead men to seek medical assistance.
Which men are affected by Benign Prostatic Hyperplasia (BPH)?
Benign Prostatic Hyperplasia (BPH) initiates in the third decade of life, in a microscopic stage (identifiable only histologically), asymptomatic.
With advancing age and the presence of androgen, around 50% of microscopic BPH will be developed in macroscopic (palpable and increased dimensions prostate).
However, clinically significant BPH in needing treatment only shows up at 50% of men over 50 years old with increased-dimensions prostates.
In the United States of America, the estimated risk of a 50-years-old man being submitted to a prostatectomy during his life is 25% to 40%. Even when not treated, a considerable number of symptomatic patients remain stable or improve without sequels.
Although the exact cause is not well-defined, one thinks that it results from interactions between the epithelium and the glandular stroma in the appropriate hormonal environment. One thinks that benign prostatic hyperplasia (BPH) is hormonal in the dependence on testosterone.
Benign Prostatic Hyperplasia (BPH) origin is mainly in the periurethral area, of the transitional zone, and is restricted to the most interior portion of the prostatic gland, that is to say: to the tissues located over the proximal urethra, the area that corresponds to approximately 2% of the overall normal prostatic volume.
How does Benign Prostatic Hyperplasia (BPH) manifest?
Symptoms usually result from ureteral obstruction.
These can be:
- Increase of urinating frequency with small urine volume, especially at night;
- Wear and/or interrupted urine jet;
- Feeling of not having emptied the bladder after urinating and/or difficulty to start urinating;
- Urgency in urinating or difficult to control urine;
- Failure in urinating, with urinary retention, resulting in catheterization;
- Blood in urine;
- Erectile dysfunction, which might be related to prostate medication.
These symptoms can occur separately or together. They might be minor, moderate, or severe. Untreated BPH can lead to severe complications: urinary retention, urinary tract infection, bladder calculi or diverticulum, and renal failure
How does Benign Prostatic Hyperplasia (BPH) cause urinary difficulties?
The Prostate can lead to the constipation of the urethra and bladder by 2 mechanisms. One by the urethral lumen stenosis for the increase of the prostatic volume (static component).
The other one is the dynamic component that consists of the smooth muscle tone, mediated by the noradrenaline effect in the adrenergic receptors found on the prostate stroma, on the prostate capsule, and the urethra.
Increasing this tone can hurry the sudden reduction of the urinary flow or even acute urinary retention, needing a catheterization. The tone can be decreased with adrenergic agonists (α-blockers), being the basis of one of the main forms of current medical therapy.
The fact that adrenergic receptors exist in other body areas explains the wide range of adverse effects frequently visible with this medication. This way, urinary complaints associated with benign prostatic hyperplasia (BPH) have two origins: anatomic and neurohormonal.
A large part of the symptoms is related to the muscular tone increase and the muscular pressure on the urethra, prostate stroma, and bladder neck through α-adrenergic receptors.
The volumetric increase with consequent anatomic compression of the urethra, which stays long and with an exaggerated posterior shape, is another essential factor. Other factors are neurotransmitters and neuroendocrine cells in the prostate tissue.
As a whole, benign prostatic hyperplasia (BPH) leads to trabeculation and hyperplasia of the detrusor muscle by chronic constipation (“urinary incontinence”), which can be accompanied by venous dilation.
What are the treatment options for Benign Prostatic Hyperplasia (BPH)?
Until a few years ago, men with Benign Prostatic Hyperplasia (BPH) and severe urinary complaints, or even urinary retention, had only two treatment options: medication and surgery.
Both prostate medication and prostate surgery have many adverse effects, namely in ejaculation and erection, with negative impacts on sexual life.
There was a lack of a minimally invasive treatment as an alternative to surgery or medication, which allowed to treat urinary complaints with fewer complications.
That was why our center developed a pioneering technique to treat patients with Benign Prostatic Hyperplasia (BPH) and urinary complaints or urinary retention – Prostatic Embolization.
Prostatic Embolization is more effective than medical treatments, has comparable effectiveness with surgery, without the complications related to it. With Prostatic Embolization, sexual function is not affected and there is a significant improvement of urinary complaints.
What are the treatment options for Benign Prostatic Hyperplasia (BPH)?
Until a few years ago, men with Benign Prostatic Hyperplasia (BPH) and severe urinary complaints, or even urinary retention, had only two treatment options: medication and surgery.
Both prostate medication and prostate surgery have many adverse effects, namely in ejaculation and erection, with negative impacts on sexual life.
There was a lack of a minimally invasive treatment as an alternative to surgery or medication, which allowed to treat urinary complaints with fewer complications.
That was why our center developed a pioneering technique to treat patients with Benign Prostatic Hyperplasia (BPH) and urinary complaints or urinary retention – Prostatic Embolization.
Prostatic Embolization is more effective than medical treatments, has comparable effectiveness with surgery, without the complications related to it. With Prostatic Embolization, sexual function is not affected and there is a significant improvement of urinary complaints.
Get in Touch.
Submit the form to schedule your appointment with Dr. Tiago.
Get in Touch.
Submit the form to schedule your appointment with Dr. Tiago.




